The Impact of Menopause on Brain Health
Menopause is a normal part of aging. It’s a major natural milestone in any woman’s life. Yet, its full effects on health often go undiscussed. While it impacts everyone differently, the link between menopause and the brain is sometimes overlooked—specifically its influence on cognitive function, mental health, energy levels, and sleep patterns.
Whether you are approaching menopause, in the midst of it, or supporting someone who is, understanding its effects on brain health can help maintain overall well-being during this transformative time. Knowing what’s happening in the mind and body can make preparing for and embracing this stage of life easier.
Join us as we uncover holistic approaches to menopause treatment to help you navigate these changes with grace and optimism.
Hormonal Changes During Menopause
As we enter menopause, the body goes through significant hormonal shifts. This natural transition marks the end of reproductive years and the start of a new chapter. Estrogen and progesterone levels fluctuate and eventually decrease, affecting many aspects of health, including brain function.
Science shows that the menopausal transition actually “reshapes the neural landscape of the female brain.” This means the brain actively adjusts to the new hormonal environment. It does this to maintain its:
- Structure
- Connections
- Energy use
- Cognitive functions
This period of change isn’t necessarily about loss or decline. Instead, it’s a time of neuroplasticity—the brain is literally rewiring itself to adapt to a new phase of life.
However, this adaptation process can certainly bring about challenges for cognitive and emotional well-being.
The Interconnected Nature of Hormonal Changes
The hormonal shifts of menopause create a ripple effect throughout the body. The same changes impacting energy levels can influence sexual health or mood stability.
The brain’s emotional response to these changes has significant influence as well. Sexual health changes can affect emotional well-being, which in turn could impact cognitive function. Similarly, changes to cognitive function might influence how one perceives and experiences their sexual health.
By recognizing that these various health changes are all due to the same transformative process, we can approach menopause with a more holistic perspective.
Cognitive Health and Menopause
Many women notice changes in their memory and concentration during menopause. You might find yourself forgetting names or misplacing items often. Mood swings and changes in mental health may occur more frequently or more intensely than before.
It’s normal to worry that these symptoms could indicate the early stages of severe cognitive decline or disorders. Rest assured, while this menopausal brain fog can be very frustrating, these experiences are common. However, this is important to note in the broader landscape of women’s brain health.

The Risk of Cognitive Decline
“Women make up an estimated 65% of people” currently living with dementia, a condition characterized by a decline in cognitive function. Researchers are still working to understand exactly why more women than men are affected. Because menopausal women demonstrate a sharper decline in memory function, it is currently believed menopause “plays a significant role in shaping memory function.”
Symptoms of menopause can be extra challenging for the brain and body, such as changes in:
- Mental health
- Sleep disturbances
- Energy levels
These factors, combined with the decrease in estrogen levels, can contribute to the brain’s increased vulnerability to damage and decline.
Keep in mind this doesn’t mean cognitive decline is inevitable for women undergoing menopause. Some menopause treatments and lifestyle changes can strengthen the brain’s resilience and well-being. Seeking a cognitive evaluation is an important step.
Assessing Cognitive Function
Some fluctuations in memory and focus are common as we age, but it’s vital to understand and assess the potential impact of menopause on the brain. There are steps you can take:
- Self-Monitoring: Pay attention to changes in memory, problem-solving skills, or ability to focus. It’s helpful to track your observations in a journal.
- Regular Medical Visits: Discuss cognitive concerns with your doctor, who can perform initial screenings and provide insights over time.
- Cognitive Assessments: Seek standardized cognitive tests, including neuropsychological evaluations and brain imaging tests, to track and rule out other causes of cognitive decline.
Early assessment can lead to better management strategies if symptoms of menopause, like brain fog and significant changes in mental health, become a major concern.
Mental Well-Being

Menopause can be an emotional rollercoaster. You might find yourself feeling irritable one moment and tearful the next or experiencing a sense of loss during this time.
There are reasons for this, such as transitioning to a new stage of life, adapting to a changing body, and feeling shifts in libido. Mood swings, anxiety, and depression are not just “in your head.” They’re real, valid responses to changes happening in the body—your brain is responding naturally to hormonal shifts.
Science shows that “menopause increases vulnerability to depression and anxiety.” This is because of the way the decrease in hormones affects important neurotransmitters responsible for regulating mood and emotions.
Seeking support is a proactive step towards taking care of yourself, but it’s also an important step in managing menopause and your brain health during this time. This may be as simple as talking to a friend or as significant as consulting with health professionals.
Reaching out can support both your emotional well-being and cognitive function.
Energy and Sleep Problems in Menopause
It’s common to feel more tired than usual. Menopause and exhaustion often go hand in hand. The associated sleep problems and overwhelming fatigue can be frustrating and draining.
Night sweats can disrupt sleep, while menopause insomnia might have you tossing and turning for hours. These sleep disturbances lead to daytime fatigue, impacting your mood and even cognitive abilities during waking hours.
The fatigue and exhaustion you might be experiencing are more than just being tired. They’re closely tied to menopause and brain health. Chronic lack of sleep inhibits the body’s capabilities over time. Research finds that, in the brain, this can result in “toxin build-up which can negatively affect the cognitive performance” in areas like:
- Memory
- Attention
- Focus
- Decision making
- Mental sharpness
Remember, menopause and its extreme fatigue do not have to be your daily reality. Addressing menopause sleep problems is important not just for your energy levels, but also for long-term brain health.

Managing Menopause Symptoms for Optimal Brain Health
Menopause brings many changes, but there are many strategies to alleviate some of the uncomfortable and concerning outcomes. Managing these changes can have a positive impact on the symptoms of menopause and brain health, including cognitive function. There is no one-size-fits-all approach to managing menopause and supporting brain health.
Hormonal Management and Brain Health
Hormone Replacement Therapy (HRT) can be an effective option for some women in alleviating menopause symptoms, including those affecting brain health. It can help with hot flashes, night sweats, and mood changes, improving sleep quality and reducing fatigue.
Like any medical treatment, HRT comes with both potential benefits and risks and can have varying effects on cognitive function:
- Potential Cognitive Benefits:
Some studies suggest that HRT, particularly when initiated near the onset of menopause, may have a beneficial effect on cognitive function in women, especially those with a genetic risk for Alzheimer’s disease (e.g., carriers of the APOE-e4 gene). It may help maintain cognitive function, including memory, attention, and verbal skills.
- Potential Cognitive Risks:
For other women, especially if HRT is initiated later in life or after a long gap post-menopause, there may be an increased risk of cognitive decline or worsening cognitive function. The timing of HRT initiation (often referred to as the “critical window hypothesis”) plays a crucial role in determining its cognitive effects.
Large clinical trials, such as the Women’s Health Initiative (WHI), have shown that HRT, particularly estrogen-progestin therapy, may be associated with an increased risk of dementia when started in women aged 65 or older.
Individual Variation:
The effect of HRT on cognition is influenced by factors such as age, the timing of therapy initiation, type of hormones used (estrogen alone vs. combined with progesterone), duration of therapy, and individual genetic makeup.
For women at genetic risk of Alzheimer’s, personalized assessment by a healthcare provider is essential to weigh the potential benefits against the risks.
Medical interventions like these are highly individual. It’s important to have an open conversation with your doctor about whether HRT is right for you, considering its potential impact on brain health.
Non-Hormonal Approaches to Brain Health
There are many other ways to approach menopause management. Other menopause treatment strategies can be used individually or in combination with lifestyle changes, depending on your specific needs and preferences. Most importantly, you feel empowered to choose menopause management strategies and support your personal health and goals.
These menopause management strategies offer different options to support your well-being in your daily life.
Lifestyle Changes
- Physical Activity: Healthy practices like exercise “can improve memory and reduce anxiety or depression.” It increases blood flow to the brain and may promote neuroplasticity.
- Nutrition: A balanced diet in brain-healthy foods, like omega-3 fatty acids, can support overall health and cognitive function during menopause.
- Stress Management: Techniques that manage stress, like meditation, yoga, and mindfulness practices, can improve sleep quality and potentially support brain health.
- Cognitive Training: Engaging in mentally stimulating activities, learning new skills, and doing challenging puzzles may offset menopause-related changes in the brain.
Homeopathy and Supplements
Some find relief from menopause symptoms through homeopathic remedies. Studies show that “quality of life improves with homeopathic treatments for hot flashes,” but more research is needed to understand the full impact on symptoms.
Certain supplements may support brain health during menopause. B-complex vitamins are beneficial, while adaptogens may help the brain “cope with different forms of stress” on your system.
Hyperbaric Oxygen Therapy (HBOT)

Hyperbaric oxygen therapy (HBOT) is an innovative treatment that involves breathing 100% pure oxygen in a pressurized environment. In combination with a holistic and personalized medical program, it’s been proven to support brain health during aging, which could be particularly relevant during the menopausal stage.
Research has shown HBOT “induced cognitive enhancements in healthy aging adults” and increased brain plasticity. It may also benefit other symptoms of menopause by potentially addressing menopause brain fog, mental health, energy levels, sleep quality, and overall well-being.
Embracing Menopause with Hope
Remember, menopause is not just an ending. It’s also a beginning—a new chapter in life filled with potential for growth and renewed vitality. As you navigate this transition, approach it with patience. Staying informed and open to menopause treatment strategies can support your brain health and overall well-being during menopause and beyond.
A holistic approach to managing menopause and the brain, potentially combining HBOT with other strategies like exercise, nutrition, and cognitive training, may offer the best support for your cognitive health during this important life transition. This is the approach at The Brain and Performance Centre, a DP World company.
Learn more about reverse aging through the holistic Brain & Performance Centre program, and contact our clinic to discover how you can approach the cognitive changes of menopause with grace and hope.

Preserve Your Cognitive Health by Understanding the Risk Factors of Alzheimer’s Disease
We all experience lapses in memory now and then, especially as we age. For most of us, these minor cognitive issues are usually just annoyances.
It is forecasted that the UAE will see an increase of 1,795 per cent with people suffering from dementia by 2050, while other Gulf countries, such as Qatar and Bahrain, will also see a very high increase in dementia cases of 1,926 percent and 1,084 per cent, respectively.
But if your cognitive issues interfere with your daily life, they could be the beginning of something much more serious. Read on to learn more about the risk factors for Alzheimer’s disease and how you can preserve your cognitive health.
What Is Alzheimer’s Disease?
Alzheimer’s disease is a form of dementia that impacts a person’s ability to think, reason, and remember. As it progresses, Alzheimer’s can severely affect quality of life, eventually becoming completely debilitating. The most common type of Alzheimer’s disease is the late-onset form, when symptoms usually become more evident in [a person’s] 6th decade of life.”
The 10 Signs and Symptoms of Alzheimer’s Disease:

According to the Alzheimer’s Association, ten early warning signs of late-onset Alzheimer’s disease include:
- Memory loss that disrupts daily life
- Challenges in planning or solving problems
- Difficulty completing familiar tasks
- Confusion with time or place
- Trouble understanding visual images and spatial relationships
- New problems with words in speaking or writing
- Misplacing things and losing the ability to retrace steps
- Decreased or poor judgment
- Withdrawal from work or social activities
- Changes in mood and personality
If you experience a cognitive problem that impacts your daily life, don’t ignore it. Dementia is not a normal part of the aging process. The sooner you seek help, the sooner you can take action against cognitive decline.
What Are Some Risk Factors for Alzheimer’s Disease?
There’s still a lot we don’t know about how Alzheimer’s disease develops or why some people are at greater risk of developing it than others. It’s an active area of study, and researchers are discovering new things every day.
The consensus among scientists is that a combination of age, sex, genetic, environmental, and lifestyle factors contribute to the development of Alzheimer’s disease.
Let’s take a closer look at some of the greatest risk factors for Alzheimer’s:
- Prevalence studies demonstrated that dementia is indeed a prevalent condition in Arab countries, ranging between 1.1% and 2.3% among age groups of 50 years and older, as well as between 13.5% and 18.5% among age groups of 80 years and above.
- “There are more women with Alzheimer’s disease than men,” though this might be because women live longer than men.
- Suffering from a traumatic brain injury (TBI) can “increase the risk of developing Alzheimer’s or another type of dementia years after the injury takes place.”
- Acute and chronic inflammation is “associated with an increase in cognitive decline in Alzheimer disease.” Eating a diet full of inflammatory foods like processed sugar might exacerbate the risk of developing inflammation in the brain.
- Exposure to environmental pollutants has been linked to an increased risk of dementia. Researchers note “half of individual differences in Alzheimer’s disease risk may be environmental.”
- Studies discovered a “significantly increased risk of Alzheimer’s disease with current smoking.” This risk factor offers another compelling reason to quit.
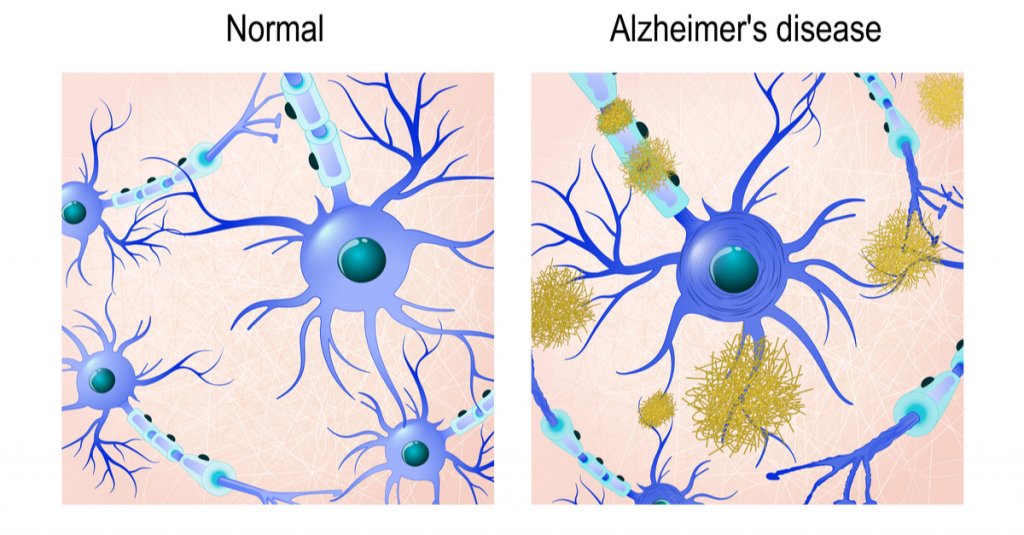
2 Protein Structures in the Brain Linked to Alzheimer’s Disease
Scientists typically focus on two different protein structures in the brain associated with Alzheimer’s disease: Neurofibrillary tangles and amyloid plaques.
It’s not currently known whether the presence of these structures causes Alzheimer’s disease or if they’re simply byproducts of it. But both can impair cognitive function and can worsen as the disease progresses.
Neurofibrillary Tangles
Neurofibrillary tangles are accumulations of a harmful protein called tau in the brain’s neurons. These tangles can inhibit the neurons’ ability to communicate, causing cognitive decline. Some studies reveal hypoxia is associated with neurofibrillary tangles.
Amyloid Plaques
Amyloid plaques are hard, insoluble clumps of beta-amyloid proteins that build up between neurons. Like neurofibrillary tangles, these plaques are toxic to brain cells and disrupt cell-to-cell communication. They can eventually result in cellular death, harming cognitive abilities even further.
New imaging technologies can reveal the presence of both protein structures, so your doctor can alert you to the presence of Alzheimer’s disease or if you’re at risk for developing it.
Is Alzheimer’s Genetic?
Both early-onset and late-onset Alzheimer’s disease have a genetic component, meaning if you have a family history of Alzheimer’s, you carry a greater risk factor for developing the disease compared to someone who doesn’t have that history.
The risk factor is greater if an immediate family member suffers from the disease, such as a parent or sibling.
Genetics are almost always the primary contributing factor of early-onset Alzheimer’s disease, which can “affect people in their 30s or 40s.”
Gene Mutations
Researchers have yet to identify any specific genes responsible for the development of late-onset Alzheimer’s.However, certain mutations of the APOE gene, which are found in chromosome 19, “[remain] the strongest, genetic risk factor for Alzheimer’s disease.” For example, the specific gene mutation APOE ε4 is linked to higher levels of amyloid plaques and is often found in people with Alzheimer’s disease.
Your doctor may order genetic testing if you have a family history of cognitive problems or early-onset dementia.
Remember, this doesn’t mean you’re destined to develop Alzheimer’s if a parent or sibling has had it. Some people who possess the APOE ε4 gene never develop Alzheimer’s disease, and some people with Alzheimer’s don’t have any gene mutations at all.
Genetics is just one of many Alzheimer’s risk factors — we still need more research to get the complete picture of what the biggest risk factor for Alzheimer’s disease is.
How Can I Prevent Alzheimer’s Disease?

A specific hyperbaric oxygen therapy (HBOT) protocol shows promise as a potential preventative measure for biomarkers of Alzheimer’s disease.
HBOT is a therapy that involves breathing 100% oxygen under increased atmospheric pressure.
- Recent research illustrates a unique HBOT protocol can shrink existing amyloid plaques in the brain and even prevent new ones from forming altogether (in animal models): Repeated sessions of HBOT showed “reduced hypoxia and neuroinflammation, reduction in beta-amyloid (Aβ) plaques and phosphorylated tau, and improvement in behavioral tasks.”
- Another study revealed HBOT improved memory recall in people who exhibited mild cognitive impairment: “HBOT should be considered as a therapeutic approach to slow the progression or even improve the pathophysiology responsible for [Alzheimer’s] disease.”
These studies offer hope that HBOT may become a viable treatment method for preventing cognitive decline.
Lifestyle Habits to Safeguard Cognitive Health
While none of us can change our genetic makeup, we can change our lifestyle. Healthy habits can help lower your risk factor for nearly any disease, not just cognitive-related conditions. Lowering inflammation levels in your body can also help lower inflammation in the brain. Some of the things you can do to preserve your cognitive health include:
- Eating a healthy diet full of fruits and vegetables
- Exercising regularly
- Maintaining healthy blood pressure
- Keeping your mind active
- Maintaining a healthy weight
- Practicing mindfulness and meditation
- Avoiding excess alcohol
- Avoiding smoking
- Getting plenty of restful sleep
- Taking care of your mental health
- Reducing stress
The Brain & Performance Centre’s Fight Against Cognitive Decline
The Brain & Performance Centre was founded on the unique Hyperbaric Oxygen protocol discussed in earlier research studies.
This protocol involves fluctuating oxygen levels during the HBOT sessions. Oxygen level variations trigger the body’s self-healing process.
Cognitive Performance and Aging Programme
The Brain & Performance Centre offers a comprehensive cognitive performance and aging programme. Our treatments are rooted in research and lean on a holistic and personalized approach.
Depending on your symptoms, needs, and goals, the programme can include the following:
- In-depth medical history review
- Comprehensive physical and neurological exam
- Physical therapy evaluation
- Highly advanced brain imaging scans
- Neurocognitive tests
During the treatment, the programme can include a combination of the following:
- Unique hyperbaric oxygen therapy session
- Cognitive training
- Physical training
- Dietary coaching
Watch Danny’s Story:
Lower Your Risk with The Brain & Performance Centre
While we still have a lot to learn about the risk factors of Alzheimer’s disease, anyone can lower their likelihood by taking charge of their lifestyle.
Preserving your cognitive health starts with the choices you make every day. Partnering with The Brain & Performance Centre brought to you by DP Worlds is just one of them.
Contact our medical team to learn how we can help you.

